- Review
- Open access
- Published:
Generating evidence on the use of Image and performance enhancing drugs in the UK: results from a scoping review and expert consultation by the Anabolic Steroid UK network
Harm Reduction Journal volume 18, Article number: 107 (2021)
Abstract
Background
The use of anabolic androgenic steroids (AAS) and associated image and performance enhancing drugs (IPEDs) is now a global phenomenon. There is a need to develop evidence to support the development of interventions to prevent the commencement of use, to minimise the potential harms or to support those in their cessation of use. While the United Kingdom (UK) is no exception to this issue, its public health and legislative response to the phenomenon differs to other countries and requires the examination of research specific to the UK. Therefore, a scoping review has been conducted to examine the recent relevant literature to help inform the development and evaluation of effective interventions to reduce the harmful use of IPEDs.
Methods
A comprehensive search strategy was developed for multiple bibliographic databases, supported by and iterative citation searching process and complimented by expert input from the Anabolic Steroid UK Network. Research conducted by or UK academics or within the UK were eligible, if published in the previous five years.
Results
In total 87 eligible outputs were identified, including 26 review articles, 25 qualitative papers and 24 quantitative papers. together with small numbers of clinical studies/case reports (6) and commentaries/correspondence (6). The most common topics of research were public health, treatment and harm reduction (41), followed by studies focusing on epidemiology, sub-groups of people using IPEDs and motivations for use (34). The studies illustrated the diverse populations of people who use a range of enhancement drugs including concomitant psychoactive drug use. A number of papers focused on blood borne viruses and associated issues, while others reported on the uptake of needle and syringe programmes. No effectiveness evaluations related to any aspect of treatment, harm reduction or other intervention were published during study period.
Conclusion
There is a need for the development of effectiveness evaluations of current interventions and any future service provision for people using image and performance enhancing drugs. While there have been no studies of this nature to date, this review illustrates the rich data that has been gathered through diverse methodologies, that will assist in the development of future effectiveness evaluations.
Background
Image and performance and enhancing drugs (IPEDs) include a wide range of drugs across various pharmacological categories. Their common features are the function of their use: the alteration of physical performance, or appearance. IPEDs [1] form a subset of human enhancement drugs (HEDs) [1,2,3], and are predominantly those that promote lean muscle mass (e.g., anabolic androgenic steroids [AAS], human growth hormone [hGH]) but may also include weight loss products such as dinitrophenol or skin tanning injections (e.g., melanotan II). Whilst the use of IPEDs is by no means a new phenomenon, until relatively recently attention has been largely restricted to professional/elite athletes and bodybuilders. However, IPED use has moved beyond the sporting arena and is now commonplace amongst non-elite, recreational trainers within mainstream gymnasia [1,2,3,4,5,6,7]. This situation is not unique to the United Kingdom (UK) and other high-income countries such as the United States of America (USA), Australia and those within Western Europe. Research has identified widespread use of IPEDs in countries across the globe [8], including countries in the Middle East [9] and South America [10, 11].
The UK is unique in its response to the use of IPEDs. In the 1990s, on the recommendation of the Advisory Council for the Misuse of Drugs, a decision was made not to criminalise the personal possession of these drugs, but to focus legislation on manufacture, distribution, and possession with intent to supply [12]. Subsequently, this principle has been maintained, with adjustments to curtail purchasing of AAS from overseas websites but no change to the legality of personal possession of AAS and associated IPEDs [13]. This approach is supported by a comprehensive network of needle and syringe programmes (NSPs) across the UK. Whilst NSPs were originally established in the 1980s in response to the HIV threat posed to people who injected heroin, people who inject IPEDs now constitute the largest client group for many NSPs in the UK [13,14,15]. The specific situation in the UK regarding the legality of AAS possession and the engagement of large numbers of people who use AAS, with a network of NSPs provides a unique backdrop to the development of effective interventions for this population. Therefore, in order to identify relevant evidence to support the development of these effectiveness evaluations it is necessary to identify collate and review the literature that is specific to the UK.
Unlike the evidence that is specific to the AAS environment in the UK, much of our knowledge in relation to the pharmacological effects of IPEDs is generalisable from research around the world and includes an increasing body of evidence highlighting physical and psychological harms stemming from AAS use. While harms to major organs and systems, in particular the heart and cardiovascular, have long been associated with the use of AAS [16], it is only over the last decade that the significance of long-term, high-dosage AAS has become apparent [17,18,19]. Alongside the recognised physical and mental health impacts, new concerning evidence is emerging in relation to long-term use being associated with structural changes to the brain, deviant brain aging, and impaired cognition. Recent studies of AAS use and the brain have also concluded that AAS dependence is associated with thinner cortex in widespread regions, specifically in prefrontal areas involved in inhibitory control and emotional regulation, compared with non-dependent AAS users [20]. Recently we have also seen greater recognition of prolonged and sometimes irreversible hypogonadism in men after long-term use of AAS [21, 22] and how the symptoms of this, including reduced libido [23], may lead to continuation or resumption of AAS use. There remains significant debate regarding the issue of aggression and violence being associated with AAS use. Recent research has concluded that for some, AAS use may contribute to aggression levels [24]. Also, while there remains the need to elucidate the mechanisms involved [25], an association between aggression and AAS dependence has been identified [26].
While the majority of people who use AAS and associated IPEDs inject at least some of these drugs [27, 28],a recent review of blood borne virus (BBV) infection amongst people who use AAS and associated IPEDs highlighted the paucity of relevant robust data globally [29]. Just nine papers published since 2000 were identified, four from the UK and Australia respectively and one from the USA. Whilst several of these studies were focused on AAS use within populations of gay and bisexual men, the large-scale UK research studies recruited AAS users from NSPs or directly from gyms. The UK study of 2010/11 identified 2% of the 395 participants as HIV positive, similar levels to those seen amongst people who inject psychoactive drugs [30]. This was supported by further data collection and analyses of surveillance data dating back to 1992, using a sample of 1296 people who had injected IPEDs. Results indicated that HIV had been present within this population for some time and provided an HIV prevalence of 1% for this period [31]. As yet we do not know the route of transmission of infection and the role that sexual contact and psychoactive drug injection may play. Furthermore, we do not know if this pattern of HIV infection amongst people who inject IPEDs is mirrored in other countries. Injection site infection and injury is a widely recognised issue. Pain and inflammation at injections sites have been identified at significant levels in studies from the UK [32], USA [33], Australia [34] and Holland [35]. While poor injecting techniques contribute to these localised infections, adulterated and contaminated products, an inevitable by-product of the illicit market is an ongoing issue on a global scale and overseas [36,37,38,39].
While AAS are the most used IPEDs, polypharmacy is the norm [7, 40]. Additional anabolic substances, such as human growth hormone (hGH) and a range of new peptide hormones (e.g., growth hormone-releasing peptide-6) are commonly used. Drugs to prevent or mitigate side-effects (e.g., tamoxifen to counter gynaecomastia), human chorionic gonadotrophin (for the resumption of normal testicular function) and a range of weight loss drugs (e.g., ephedrine, dinitrophenol, clenbuterol) are also part of the established pharmacopeia. Low-cost production and distribution, combined with the increasing sourcing routes via the internet has resulted in substances that were once prohibitively expensive now being commonplace [41]. Furthermore, the use of other human enhancement drugs including melanotan II and sildenafil combined with psychoactive drugs is prevalent amongst some cohorts who use IPEDs, sometimes with significant potential for harmful interactions with certain drugs (e.g., cocaine) [42].
People who use AAS and associated IPEDs are by no means a homogenous group. Recent work has highlighted various typologies of user comprised of multiple subgroups with varied characteristics, risk behaviours and levels of engagement with support services [43,44,45]. While the focus of much of the research has centred on male use of these substances use, women do use IPEDs and in some cases use AAS, for those women using AAS the potential harms are more significant and sometimes compounded by an added sense of stigma and reluctance to engage with support services or healthcare [46].
The need for evidence to support our understanding of interventions that can reduce the harmful use of IPEDs is increasingly recognised (e.g. [47, 48]). As attention from the research community on IPEDs has amplified substantially in recent decades [15], the enlarged evidence base may provide valuable insights that will support those working to reduce harm amongst people who use IPEDs and ensure that approaches are based on a thorough understanding of up to date evidence. The review therefore sought to identify and explore evidence that will support the development and evaluation of effective interventions to reduce the harmful use of IPEDs. The underpinning research question developed by the research team was “how has the academic literature base on the use of IPEDs in the UK developed in the past five years and what does it tell us?”. Specifically, we sought to gain insight into the characteristics of studies investigating IPED use including: the methods used, topics of research, the characteristics of study populations, and key themes within study findings and recommendations. We conducted a scoping review of UK literature on the use of IPEDs to map and describe extant UK based literature, and in partial fulfilment of the UK National Institute for Health Research development grant (NIHR 132730), Image and Performance Enhancing Drugs (IPEDs): Assessment of available intelligence and research gaps to inform intervention evaluation’ [47]. While the international evidence base pertaining to the pharmacological effects of AAS and associated IPEDs is largely applicable to the UK, the specific situation in the UK warranted a review of the UK published literature over the last five years. It is within this environment that we sought to identify the current research landscape to ultimately inform the development of evidence based effective interventions. Therefore, this review looked specifically at the AAS/IPED outputs from UK academics/institutions. These results compliment related NIHR research activity comprising estimations of the size of the population of people who use AAS, the extent and characteristics of service provision for this group and the systems mapping of factors that influence the harmful use of IPEDs.
Methodology
Approach
A scoping review design was chosen to map and describe what is known about the current status and focus of research in relation to IPEDs in the UK. Scoping reviews were first proposed by Arksey and O'Malley [49] and have been further advanced by others over the last decade [50,51,52]. More recently, Tricco, Lillie [53] defined scoping reviews as “a type of knowledge synthesis, follow a systematic approach to map evidence on a topic and identify main concepts, theories, sources, and knowledge gaps”. This independent research methodology addresses broader research questions than systematic reviews can answer [49,50,51,52]. Scoping reviews are generally conducted to identify knowledge gaps, examine the extent (i.e. size), range (i.e. variety), and nature (i.e. characteristics) of a specific topic, summarise the findings of a heterogeneous body of knowledge, and propose agendas for future policy and research [49, 52, 54, 55].
Search strategy
Arksey and O'Malley [49] five-stage iterative scoping review methodology was adhered to, namely: [1] identifying the essential research question, [2] identifying relevant studies, [3] study selection, [4] charting the data, and [5] collecting, summarising, and reporting the results. A search was undertaken in January 2021, in Liverpool John Moores University Library catalogues using the following databases: Web of Science; MEDLINE; Science Direct; PsycINFO; SPORTDiscus; CINHAL Plus; PubMed; Google Scholar, and Google. Search terms were compiled and agreed by the research team who had extensive knowledge and experience of public health, addiction, and IPED research (see Table 1).
Study selection
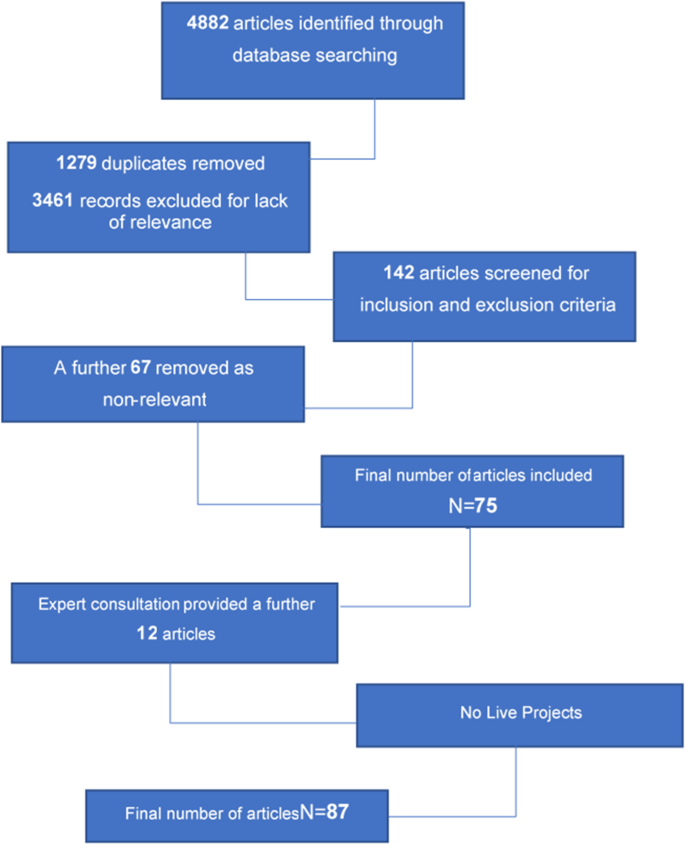
The initial search identified 4,882 articles based on the search terms outlined above (see Table 1), References were imported to Endnote® citation manager where they were organised. An initial examination of the articles indicated the possibility of many irrelevant articles. Duplicates were removed (n = 1279) followed by title and abstract screening of the remainder (n = 3461), where inclusion and exclusion criteria were applied to all citations. Studies included were: all published empirical research including articles in peer-reviewed journals and book chapters; and grey literature such as national policy reports and documents, needs assessments, service evaluations, and locally commissioned research. Date range was restricted to between January 1st 2016 and December 31st 2020 to capture current, relevant literature to inform the development and evaluation of effective interventions to reduce harmful IPED use, and studies conducted by UK academics or those with a UK focus due to the unique situation in the UK relating to legislation and NSP provision. Academic theses, animal models, and in-vitro studies were excluded. A total of 77 records were identified at this stage of the search (see Fig. 1). Papers were subsequently reviewed and screened to ensure those included met the inclusion criteria and discrepancies resolved [54]. Manual searching of the reference lists of the 77 records was conducted to identify any relevant literature that was not captured in the initial search. Subsequently, consultation with academics and healthcare professionals with relevant expertise (accessed through the Academic Steroid UK Network) was conducted to ensure all relevant literature was included, as recommended by Daudt, van Mossel [54]. This was a valuable step in the process as the depth and breadth of knowledge each expert brought strengthened the review and consequently, the richness of the findings. A final number of 87 sources were included in the review (see Fig. 1).
Data extraction and charting
Data were extracted to form a dataset which included all author names and institutions, year of publication, aim and method, population, key findings, implications for policy and practice, and identified research gaps in each source.
Results
Additional file 1: Table 2 provides a detailed overview of UK academic publications on the use of anabolic androgenic steroids and IPEDs, presenting an overview of this research to illustrate its volume and main characteristics, together with summaries of key findings.
Profile of studies reviewed
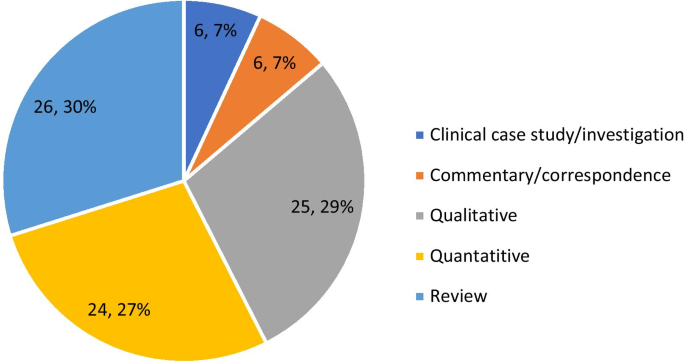
The final sample of 87 records present a range of methodologies and foci on AAS and other IPEDs within the UK. The majority of evidence was gleaned from the review of 69 journal articles and supplemented by 12 relevant academic book chapters and six public health reports. There is no discernible trend in the volume, methodologies used or focus of research outputs over the five-year period. Apart from 2019, the number of outputs per year ranged between 12 and 17 publications. The high number of outputs in 2019 [29] can be explained by the inclusion of 8 chapters from one book on the use of human enhancement drugs [1]. These records are comprised of a variety of methodologies and approaches including qualitative, quantitative and review. In a small minority of cases several methods were reported within the research output, however in all cases there was a clear predominant method applied. For example, the book chapter ‘The supply of image and performance enhancing drugs (IPED) to local non-elite users in England [56], forensic analysis of a small number IPEDs was used to support the findings of two qualitative studies and was therefore recorded as a qualitative paper. Figure 2 illustrates these methodologies in an aggregated form. The 26 review articles (including systematic, scoping, and non-specific reviews) account for the largest proportion of outputs(30%), followed by 25 predominantly qualitative (29%), 24 quantitative papers (27%) with 6 (7%) commentary papers and clinical case studies respectively.
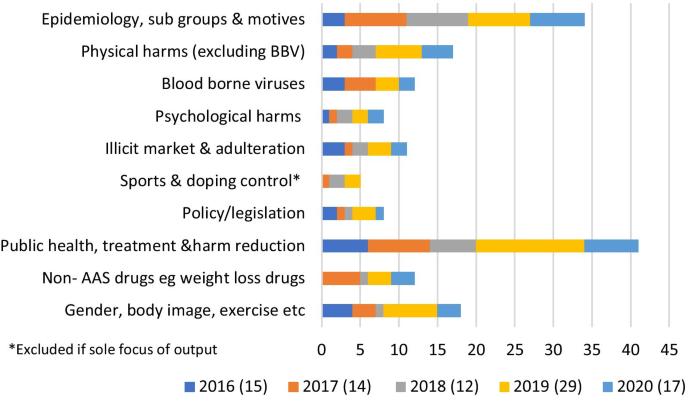
Additional file 1: Table 2 also includes the main topics of each output. It is important to note that while the category of sport/doping control is included, outputs were excluded if this was the sole area of focus. Outputs may be attributed to two are more categories. Figure 3 summarises these categories within the year of publication. The most common topic of research, included in 41 academic outputs, was public health/care (including harm reduction and treatment). This was consistent across each year apart from 2018 when epidemiology was the major category, this being the second most common topic overall [34].
Key findings
The UK research from the last 5-years provided a broad spectrum of evidence related to various facets of IPED use, from across the full extent of the UK. An indication of the diversity of drugs used is provided, together with specific implications. The vast majority of the work was in relation to the use of AAS includingone paper looking at the concomitant use of stimulants [42] Four papers focusing solely on the use of weight loss drugs [57,58,59,60], two papers examining the use of the skin tanning drug melanotan [61, 62], two academic outputs describing the emerging use of the respective peptide hormones metformin and CJC-1295 [63, 64], and one article examining the use of synthol (a site enhancement oil) [65]. One paper focused specifically onthose solely taking oral AAS and associated drugs [66], two papers examined the relationshipbetween supplements IPED use [67, 68], whilethe role of concomitant psychoactive drugs was emphasised as a cause for concern in one paper [7]. Six outputs provided accounts of the ease of availability and affordability of drugs within a dynamic IPED market [56, 69,70,71,72,73], with the internet playing an important role with a significant market crossover with other drug using populations [74,75,76,77].
Research focused on epidemiology, sub-groups, and motives, indicates a complex landscape of diverse sub-populations of IPED users, going beyond the stereotypical young male AAS user. Different populations and practices were identified with specific practices and risks. Significant sub-groups included women using a range of substances [78,79,80,81,82] and older men using AAS [28]. While research that only focused on elite sport and doping control was excluded, sport clearly plays a significant role in the use of IPEDs [83] and remains a public policy concern [84]. IPED use was also associated with specific occupations as diverse as those in the military to those engaged in dance [85, 86]. The majority of the literature in this review examined the use of AAS, in particular the use of AAS by men. Only four papers solely focused on the use of IPEDs by women [57, 64, 78, 81].
This literature also provides an improved understanding of some of the motives for commencement of use or abstinence, in particular those related to self-esteem, body image and masculinity [87,88,89,90,91,92,93,94,95,96]. The continuation or resumption of AAS use driven by symptoms of hypogonadism [97,98,99,100] was a significant finding, together with wider issues related to sexual health [101]. Harms associated with IPED use were commonly described [18, 19, 102, 103], together with the risk environment [6] and efforts by individuals to mitigate these adverse consequences [104].
Common features within studies centred on public health, treatment, and harm reduction included the increasing number of AAS users engaging with NSPs [28, 105, 106] and barriers to service engagement including a lack of confidence in practitioners’ knowledge, perceived stigma. A failure to recognise the beneficial effects of AAS was identified together with an overemphasis of the harms [107,108,109,110], while the need for non-judgemental specialised services was emphasised [111,112,113,114,115,116,117,118,119]. A greater understanding of the need for a multi-layered approach to preventing both IPED use in general, and harmful use in particular, was emphasised [91, 120, 121]. The need for an understanding of the culture as well as the behaviours of people who use IPEDs was deemed essential, together with an appreciation that IPEDs may have potential benefits to the user [58, 108, 110].
Another recurring theme within this literature was the need for health practitioners to demonstrate both a non-judgemental attitude and have a demonstrable level of knowledge of both IPEDs and how they are used. This was considered a prerequisite if the current barriers to service engagement are to be overcome [110]. Practitioners must have an appreciation of the complex relationship between AAS use and body image [96] and an understanding that there is a perceived normalisation of IPED use within some social groups, with concepts around masculinity and muscularity being highly influential on decisions to use IPEDs [91]. While the majority of the literature referred to practitioners in general, the potential for an increased role for both social workers [115] and endocrinologists [116] was highlighted.
Various aspects of a potential continuum of care and support were also discussed. These ranged from prevention activities within a generic health promotion approach, recognising the complex factors that make children, youth and adults vulnerable to IPEDs [42, 120, 121], through to the need for relapse prevention to divert former AAS users from a focus on their body as their major source of self-esteem [94]. However, the main area of discussion related to existing and potential harm reduction interventions and services [7, 15, 111]. In addition to the expansion of innovative development and activity within NSPs [107, 122], other venues and modes of engagement to promote sexual health [101] and ensure non-stigmatising environments were called for [28, 29, 123, 124]. There were also calls for the implementation of effective assertive outreach [125] and the adjustment of health and social care settings to enhance on-site engagement with people who use IPEDs [107].
As part of service provision there were also calls for comprehensive testing including physiological indicators of harm [112] together with testing for BBVs [126] and psychosocial support regarding body image. Such testing for BBVs could draw upon the improved understanding of injecting beliefs and behaviours [101], including BBV risks [25, 27, 102,103,104,105,106,107], evident in the review. Information of nutrition and exercise [113], building self-esteem [97], psychological services to address dependence and muscle dysmorphia [82, 97], and other body image vulnerabilities [59] were also considered necessary. There were consistent findings regarding the need for practitioners to have an understanding of the diverse populations of people who use IPEDS [45], the episodic nature of use [74], polydrug use [7], those who do not inject [66] and those using drugs other than AAS [58, 60, 127]. An understanding of the market was considered necessary in order to provide credible health related information on risks of active ingredients and the quality products obtained through the illicit market [64].
Discussion
The diversity of UK published research between 2016 and 2020 reflects a growing scientific and academic interest in this phenomenon and underpins the complex issues related to the use of available IPEDs. They also indicate the multidisciplinary response that is required if, as researchers, practitioners, policy makers, and all importantly, people who use these drugs, are going to synergise and work collaboratively to raise awareness increase our understanding and ultimately reduce the harms associated with use. The research findings, together with the stated implications for policymakers, practitioners and the research community illustrate the broad spectrum of opportunities to reduce harm, including prevention, diversion, treatment, cessation support and policies that directly affect the illicit market. However, notable by their absence and as highlighted within many of the publications is the lack of robust effectiveness of evaluations in relation to interventions focused on the use of IPEDs. While the focus of this paper is on recently published UK research, due to the unique position we are in, in relation to legislation and needle and syringe provision, it is worth noting that this dearth of intervention effectiveness evidence is replicated around the globe.
Findings also underscore the need for future efforts to develop and evaluate interventions should see the involvement of people who use IPEDs as an essential component during all stages of the research process. For example, many included records emphasised that interventions should encompass peer support groups and educators [113, 125], and a client-centred approach [79, 106]. Thus, there was a recurring theme within the UK literature of the recognition of the need to effectively engage with the communities of people who use IPEDs. It is a widely held belief that the required interventions and the research that is needed to test and evaluate them can only be achieved with the participation of those who use IPEDs. This belief is supported not only by the IPED-specific literature reviewed here, but also by the broader literature relevant to the development and evaluation of interventions aimed at enhancing or protecting physical and psychological health. Often referred to as patient and public involvement (PPI), research funders now frequently endorse and sometimes obligate PPI during all stages of health and social care research [129, 130]. Incorporating PPI can benefit research by promoting recruitment [131], which can enhance its validity and reduce costs [132]. Moreover, the efficacy of PPI is greatest when those with lived experience of the behaviour/condition being studied are represented as research partners, supporting the benefits of harnessing knowledge from such experience-based experts alongside that of scientists and professionals when designing, delivering, and disseminating research [133]. The importance of involving those with lived experience of IPED use in research and in developing and evaluating harm reduction interventions for IPED use is perhaps even more important than in other fields given evidence demonstrating a lack of trust in healthcare professionals when it comes to IPED use [134–136].
The research literature provided a wealth of far-reaching recommendations for future research. It is essential that researchers engage and collaborate with the communities of people who use IPEDs to better understand the patterns of drug-use behaviours, motives and associated risks [28]. Future research should focus on delivery of holistic healthcare and early intervention for those attending NSPs and outreach services [42]. However, harm reduction should look beyond NSPs to meet the needs of those who do not inject [66].
While the evidence base related to harms stemming from AAS use has developed over the last 5 years, there needs to be a continued focus on specific adverse effects for the full range of IPEDs [18, 19, 65, 117, 123], so that policy makers have a comprehensive understanding of the drivers and motives for use and cessation, and the associated harms for AAS [6, 79, 91, 114, 117, 124] and other IPEDs [15, 57,58,59,60,61, 64, 68, 73, 104, 122, 128]. We should also develop the evidence and increase our understanding of the issues associated with the diverse populations that use IPEDs [95, 105]. More specifically, research should focus on those people using IPEDs who may be particularly vulnerable [76], including women [78, 81], those in prison [117], those with specific occupations and those engaging in pertinent activities such as sport [67, 83, 85, 86, 90, 93].
Motives for commencement, continuation, and potential cessation of IPED use should also receive continued research attention [92, 98, 120]. Key examples identified for further attention include body image [96, 97, 129], muscle dysmorphia [94], muscularity [82], masculinity [87, 130], and hypogonadism [99, 113, 115]. Research findings indicate a combination of routinely available data, survey data and other novel data collection methods should be employed [95], including online methodologies to gain a better understanding of the prevalence of use and associated behaviours [15, 45, 64, 74, 116, 127]. Research is also needed into the clinical treatment of adverse effects [102] and how stigma and barriers within generic health services may be effectively addressed [112]. This is especially pertinent in relation BBV services [28, 31, 119, 126, 131, 132] and sexual health services [31], including men who have sex with men and women who have sex with women [101]. We also need to gain a better understanding of the supply and distribution of IPED, the role of the internet, potential for a more regulated market and the harms caused by the illicit market [6, 7, 15, 63, 69, 73,74,75]. The overarching them in relation to identified research gaps and recommended focus of attention is the evaluation of interventions to identify cost-effective demand reduction and harm reduction solutions [104, 105, 107, 111, 128]. Further attention is warranted by policymakers and public health surveillance systems to track and monitor this emerging and increasingly mainstream form of body modification and consumerism of IPED pharmaceuticals.
Conclusion
The UK IPED research community has been highly active over the last five years. This review evidences a wealth of data relating to people who use IPEDs, including their practices and associated harms. However, where interventions are a focus of the research, findings tend to be descriptive and their remains a paucity of effectiveness studies. The literature highlights the need for meaningful involvement of people with lived experience, reinforcing the principles of co-production in the development of future intervention evaluations to reduce the harms associated with this form of substance use.
References
Van de Ven K, Mulrooney KJ, McVeigh J. Human enhancement drugs. 1st ed. Abigdon: Routledge; 2019.
Evans-Brown M, McVeigh J, Perkins C, Bellis M. Human enhancement drugs: the emerging challenges to public health. Liverpool: North West Public Health Observatory; 2012.
McVeigh J, Evans-Brown M, Bellis MA. Human enhancement drugs and the pursuit of perfection. Adicciones. 2012;24(3):185–90.
McVeigh J, Begley E. Anabolic steroids in the UK: an increasing issue for public health. Drugs Educ Prevent Policy. 2017;24(3):278–85.
Coomber R, Pavlidis A, Santos GH, Wilde M, Schmidt W, Redshaw C. The supply of steroids and other performance and image enhancing drugs (PIEDs) in one English city: fakes, counterfeits, supplier trust, common beliefs and access. Perform Enhanc Health. 2014;3(3):135–44.
Hanley Santos G, Coomber R. The risk environment of anabolic-androgenic steroid users in the UK: examining motivations, practices and accounts of use. Int J Drug Policy. 2017;40:35–43.
Salinas M, Floodgate W, Ralphs R. Polydrug use and polydrug markets amongst image and performance enhancing drug users: implications for harm reduction interventions and drug policy. Int J Drug Policy. 2019;67:43–51.
Sagoe D, Pallesen S. Androgen abuse epidemiology. Curr Opin Endocrinol Diabetes Obes. 2018;25(3):185–94.
Hearne E, Wazaify M, Van Hout MC, Atkinson A, McVeigh J. Anabolic-androgenic steroid use in the Eastern Mediterranean region: a scoping review of extant empirical literature. Int J Mental Health Addict. 2020;19:1162–89.
de Siqueira Nogueira FR, de Freitas BA, de Oliveira CVC, Vieira TI, Beniz Gouveia RL. Anabolic–androgenic steroid use among Brazilian bodybuilders. Subst Use Misuse. 2014;49(9):1138–45.
Abrahin OSC, de Sousa EC, Santos AM. Prevalence of the use of anabolic-androgenic steroids in Brazil: A systematic review. Subst Use Misuse. 2014;49(9):1156–62.
Druglink. ACMD recommends new controls on steroids. Druglink. 1993;September/October 1993.
ACMD. Consideration of the Anabolic Steroids. London (UK); 2010.
Kimergard A, McVeigh J. Variability and dilemmas in harm reduction for anabolic steroid users in the UK: a multi-area interview study. Harm Reduct J. 2014;11(ARTN 19):19.
McVeigh J, Begley E. Anabolic steroids in the UK: an increasing issue for public health. Drug-Educ Prev Polic. 2017;24(3):278–85.
Hartgens F, Kuipers H, Wijnen JAG, Keizer HA. Body composition, cardiovascular risk factors and liver function in long term androgenic-anabolic steroids using bodybuilders three months after drug withdrawal. Int J Sports Med. 1996;17(6):429–33.
Baggish AL, Weiner RB, Kanayama G, Hudson JI, Lu MT, Hoffmann U, et al. Cardiovascular toxicity of illicit anabolic-androgenic steroid use. Circulation. 2017;135(21):1991–2002.
Angell PJ, Green DJ, Lord R, Gaze D, Whyte G, George KP. Acute cardiovascular responses to resistance exercise in anabolic steroids users: a preliminary investigation. Sci Sports. 2018;33(6):339–46.
McCullough D, Webb R, Enright KJ, Lane KE, McVeigh J, Stewart CE, et al. How the love of muscle can break a heart: Impact of anabolic androgenic steroids on skeletal muscle hypertrophy, metabolic and cardiovascular health. Rev Endocr Metab Disord. 2020;22(2):389–405.
Hauger LE, Westlye LT, Fjell AM, Walhovd KB, Bjornebekk A. Structural brain characteristics of anabolic-androgenic steroid dependence in men. Addiction. 2019;114:1405–15.
Kanayama G, Kaufman MJ, Pope HG. Public health impact of androgens. Curr Opin Endocrinol. 2018;25(3):218–23.
Pope HG Jr, Wood RI, Rogol A, Nyberg F, Bowers L, Bhasin S. Adverse health consequences of performance-enhancing drugs: an Endocrine Society scientific statement. Endocr Rev. 2014;35(3):341–75.
Harvey O, Parrish M, van Teijlingen E, Trenoweth S. Libido as a motivator for starting and restarting non-prescribed anabolic androgenic steroid use among men: a mixed-methods study. Drug-Educ Prev Polic. 2021. https://doi.org/10.1080/09687637.2021.1882940.
Chegeni R, Pallesen S, McVeigh J, Sagoe D. Anabolic-androgenic steroid administration increases self-reported aggression in healthy males: a systematic review and meta-analysis of experimental studies. Psychopharmacology (Berl). 2021. https://doi.org/10.1007/s00213-021-05818-7.
Pope HG, Jr., Kanayama G, Hudson JI, Kaufman MJ. Review article: anabolic-androgenic steroids, violence, and crime: two cases and literature review. Am J Addict. 2021;30(5):423–32.
Hauger LE, Havnes IA, Jorstad ML, Bjornebekk A. Anabolic androgenic steroids, antisocial personality traits, aggression and violence. Drug Alcohol Depend. 2021;221:108604.
Bonnecaze AK, O’Connor T, Aloi JA. Characteristics and attitudes of men using anabolic androgenic steroids (AAS): a survey of 2385 men. Am J Mens Health. 2020;14(6):1557988320966536.
Begley E, McVeigh J, Hope V, Bates G, Glass R, Campbell J, et al. Image and performance enhancing drugs: 2016 National Survey Results. Liverpool: Liverpool John Moores University; 2017.
Hope V, Iversen J. Infections and risk among people who use image and performance enhancing drugs. In: Van de Ven K, Mulrooney K, McVeigh J, editors. Humam enhancement drugs. Abingdon: Routledge; 2019.
Hope VD, McVeigh J, Marongiu A, Evans-Brown M, Smith J, Kimergard A, et al. Prevalence of, and risk factors for, HIV, hepatitis B and C infections among men who inject image and performance enhancing drugs: a cross-sectional study. BMJ Open. 2013;3(9):e003207.
Hope VD, Harris R, McVeigh J, Cullen KJ, Smith J, Parry JV, et al. Risk of HIV and hepatitis B and C over time among men who inject image and performance enhancing drugs in england and wales: results from cross-sectional prevalence surveys, 1992–2013. J Acquir Immune Defic Syndr. 2016;71(3):331–7.
Hope VD, McVeigh J, Marongiu A, Evans-Brown M, Smith J, Kimergard A, et al. Injection site infections and injuries in men who inject image- and performance-enhancing drugs: prevalence, risks factors, and healthcare seeking. Epidemiol Infect. 2015;143(1):132–40.
Ip EJ, Barnett MJ, Tenerowicz MJ, Perry PJ. The anabolic 500 survey: characteristics of male users versus nonusers of anabolic-androgenic steroids for strength training. Pharmacotherapy. 2011;31(8):757–66.
Larance B, Degenhardt L, Copeland J, Dillon P. Injecting risk behaviour and related harm among men who use performance- and image-enhancing drugs. Drug Alcohol Rev. 2008;27(6):679–86.
Smit DL, Buijs MM, de Hon O, den Heijer M, de Ronde W. Positive and negative side effects of androgen abuse. The HAARLEM study: a one year prospective cohort study in 100 men. Scand J Med Sci Sports. 2020;30(3):531–39.
Fabresse N, Gheddar L, Kintz P, Knapp A, Larabi IA, Alvarez JC. Analysis of pharmaceutical products and dietary supplements seized from the black market among bodybuilders. Forensic Sci Int. 2021;322:110771.
Cho SH, Park HJ, Lee JH, Do JA, Heo S, Jo JH, et al. Determination of anabolic-androgenic steroid adulterants in counterfeit drugs by UHPLC-MS/MS. J Pharm Biomed Anal. 2015;111:138–46.
Evans-Brown M, Kimergard A, McVeigh J. Elephant in the room? The methodological implications for public health research of performance-enhancing drugs derived from the illicit market. Drug Test Anal. 2009;1(7):323–6.
Ribeiro MVD, Boralle N, Felippe LG, Pezza HR, Pezza L. H-1 NMR determination of adulteration of anabolic steroids in seized drugs. Steroids. 2018;138:47–56.
Sagoe D, McVeigh J, Bjornebekk A, Essilfie MS, Andreassen CS, Pallesen S. Polypharmacy among anabolic-androgenic steroid users: a descriptive metasynthesis. Subst Abuse Treat Prev Policy. 2015;10(ARTN 12):12.
Evans-Brown M, McVeigh J. Injecting human growth hormone as a performance-enhancing drug-perspectives from the United Kingdom. J Subst Use. 2009;14(5):267–88.
Zahnow R, McVeigh J, Bates G, Winstock AR. Motives and correlates of anabolic-androgenic steroid use with stimulant polypharmacy. Contemp Drug Probl. 2020;47(2):118–35.
Christiansen AV. Gym culture, identity and performance-enhancing drugs: tracing a typology of steroid use. Oxon: Routledge; 2020.
Christiansen AV, Vinther AS, Liokaftos D. Outline of a typology of men’s use of anabolic androgenic steroids in fitness and strength training environments. Drugs Educ Prevent Policy. 2016;24(3):295–305.
Zahnow R, McVeigh J, Bates G, Hope V, Kean J, Campbell J, et al. Identifying a typology of men who use anabolic androgenic steroids (AAS). Int J Drug Policy. 2018;55:105–12.
Havnes IA, Jorstad ML, Innerdal I, Bjornebekk A. Anabolic-androgenic steroid use among women—A qualitative study on experiences of masculinizing, gonadal and sexual effects. Int J Drug Policy. 2020:102876. https://doi.org/10.1016/j.drugpo.2020.102876.
McVeigh J. Application Development Award Image and Performance Enhancing Drugs (IPEDs): Assessment of available intelligence and research gaps to inform intervention evaluation: NIHR; 2021 [Available from: https://www.journalslibrary.nihr.ac.uk/programmes/phr/NIHR132730/#/.
Bates G, Shepherd S, McVeigh J. Harm reduction strategies for androgen users: providing appropriate support and improving engagement with healthcare. Curr Opin Endocrinol Diabetes Obes. 2021. https://doi.org/10.1097/MED.0000000000000676.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Khalil H, Peters M, Godfrey CM, McInerney P, Soares CB, Parker D. An evidence-based approach to scoping reviews. Worldviews Evid Based Nurs. 2016;13(2):118–23.
Peters MDJ, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Daudt HML, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med Res Methodol. 2013;13(1):48.
Tricco AC, Lillie E, Zarin W, O’Brien K, Colquhoun H, Kastner M, et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med Res Methodol. 2016;16:15.
Coomber R, Salinas M. The supply of image and performance enhancing drugs (IPED) to local non-elite users in England: Resilient traditional and newly emergent methods. Human enhancement drugs. Abingdon: Routledge; 2019.
Germain DJ, Leavey DC, Van Hout PMC, McVeigh PJ. 2,4 dinitrophenol: It's not just for men. Int J Drug Policy. 2020:102987. https://doi.org/10.1016/j.drugpo.2020.102987.
McVeigh J, Germain J, Van Hout MC. 2,4-Dinitrophenol, the inferno drug: a netnographic study of user experiences in the quest for leanness. J Subst Use. 2017;22(2):131–8.
Germain J, McLean C, Leavey C. One size does not fit all: Tackling the issue of weight-loss drug use. In: van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Ainsworth NP, Vargo EJ, Petroczi A. Being in control? A thematic content analysis of 14 in-depth interviews with 2,4-dinitrophenol users. Int J Drug Policy. 2018;52:106–14.
Van Hout MC, McVeigh J. The use of sunless synthetic tanning products. In: Van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Dreyer BA, Amer T, Fraser M. Melanotan-induced priapism: a hard-earned tan. BMJ Case Rep. 2019;12(2):e227644. https://doi.org/10.1136/bcr-2018-227644
Graham MR, Baker JS, Davies B. Peptide hormones, metformin and new-wave practices and research therapies. In: Hall M, Grogan S, Gough B, editors. Chemically modified bodies. London: Palgrave Macmillan; 2016.
Van Hout MC, Hearne E. Netnography of female use of the synthetic growth hormone CJC-1295: pulses and potions. Subst Use Misuse. 2016;51(1):73–84.
Hall M, Grogan S, Gough B. Bodybuilders’ accounts of synthol use: The construction of lay expertise online. J Health Psychol. 2016;21(9):1939–48.
van de Ven K, Zahnow R, McVeigh J, Winstock A. The modes of administration of anabolic-androgenic steroid (AAS) users: are non-injecting people who use steroids overlooked? Drug Educ Prev Policy. 2019;27(2):131–5.
Boardley ID. Licit forms of performance enhancement and possible links with IPED use: Current knowledge and future directions. In: Van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Mooney R, Simonato P, Ruparelia R, Roman-Urrestarazu A, Martinotti G, Corazza O. The use of supplements and performance and image enhancing drugs in fitness settings: A exploratory cross-sectional investigation in the United Kingdom. Hum Psychopharmacol Clin Exp. 2017;32:e2619. https://doi.org/10.1002/hup.2619.
Turnock LA. Inside a steroid ‘brewing’ and supply operation in South-West England: An ‘ethnographic narrative case study.’ Perform Enhancem Health. 2020;7:3–4.
Hall A, Antonopoulos GA. The (online) supply of illicit lifestyle medicines: a criminological study. In: Van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Coomber-Moore J. An exploration of evolving forms of access to performance and image enhancing drugs (PIED), and body image, on Gold Coast, Australia, with particular emphasis on how users reconcile their drift into criminality. Essex: University of Essex; 2017.
Hall A, Koenraadt R, Antonopoulos GA. Illicit pharmaceutical networks in Europe: organising the illicit medicine market in the United Kingdom and the Netherlands. Trends Organ Crime. 2017;20(3–4):296–315.
Hall A, Antonopoulos A. Fake meds online the internet and the transnational market in illicit pharmaceuticals. London: Palgrave Macmillan; 2016.
Tay Wee Teck J, McCann M. Tracking internet interest in anabolic-androgenic steroids using Google Trends. Int J Drug Policy. 2018;51:52–5.
Antonopoulos GA, Hall A. “Gain with no pain’’: anabolic-androgenic steroids trafficking in the UK.” Eur J Criminol. 2016;13(6):696–713.
Chatwin C, Measham F, O’Brien K, Sumnall H. New drugs, new directions? Research priorities for new psychoactive substances and human enhancement drugs. Int J Drug Policy. 2017;40:1–5.
McVeigh J, Salinas M, Ralphs R. A sentinel population: The public health benefits of monitoring enhanced body builders. Int J Drug Policy. 2020:102890. https://doi.org/10.1016/j.drugpo.2020.102890.
Kotzé J, Richardson A, Antonopoulos GA. Looking ‘acceptably’ feminine: A single case study of a female bodybuilder’s use of steroids. Perform Enhanc Health. 2020;8:2–3.
Richardson A, Dixon K, Kean J. Superheroes—Image and performance enhancing drug (IPED) use within the UK, social media and gym culture. J Forensic Leg Med. 2019;64:28–30.
Richardson A, Antonopoulos GA. Anabolic-androgenic steroids (AAS) users on AAS use: Negative effects, “code of silence”, and implications for forensic and medical professionals. J Forensic Leg Med. 2019;68:101871.
Henning A, Andreasson J. "Yay, Another Lady Starting a Log!": Women's Fitness Doping and the Gendered Space of an Online Doping Forum. Commun Sport. 2019. https://doi.org/10.1177/2167479519896326.
Harris MA, Dunn M, Alwyn T. Symptoms of muscle dysmorphia between users of anabolic androgenic steroids with varying usage and bodybuilding experience. Eur J Health Psychol. 2019;26(1):21–24.
UKAD. Image and performance enhancing drugs. London: UK Anti-Doping; 2019.
Chester N, McVeigh J. Drug use in society and the impact on the anti-doping movement. In: Mottram DR, Chester N, editors. Drugs in Sport. London: Routledge; 2018.
Whyte I, Pattinson E, Leyland S, Soos I, Ling J. Performance and image enhancing drugs use in active military personnel and veterans: A contemporary review. Transl Sports Med. 2020;4(1):72–87.
Boardley ID, Allen N, Simmons A, Laws H. Nutritional, medicinal, and performance enhancing supplementation in dance. Perform Enhanc Health. 2016;4(1–2):3–11.
Cranswick I, Richardson D, Littlewood M, Tod D. “Oh take some man-up pills”: A life-history study of muscles, masculinity, and the threat of injury. Perform Enhanc Health. 2020;8:2–3.
Kotze J, Antonopoulos GA. Boosting bodily capital: Maintaining masculinity, aesthetic pleasure and instrumental utility through the consumption of steroids. J Consumer Cult. 2019;21(3):683–700.
Corazza O, Simonato P, Demetrovics Z, Mooney R, van de Ven K, Roman-Urrestarazu A, et al. The emergence of Exercise Addiction, Body Dysmorphic Disorder, and other image-related psychopathological correlates in fitness settings: A cross sectional study. PLoS ONE. 2019;14(4):e0213060.
Boardley ID, Smith AL, Mills J, Grix J, Wynne C, Wilkins L. Development of moral disengagement and self-regulatory efficacy assessments relevant to doping in sport and exercise. Psychol Sport Exerc. 2018;36:57–70.
Bates G, Tod D, Leavey C, McVeigh J. An evidence-based socioecological framework to understand men’s use of anabolic androgenic steroids and inform interventions in this area. Drugs Educ Prev Policy. 2018;26(6):484–92.
Harris M, Dunn M, Alwyn T. Intrasexual competition as a potential influence on anabolic-androgenic steroid use initiation. J Health Psychol. 2017;24(9):1210–20.
Boardley ID, Smith AL, Mills JP, Grix J, Wynne C. Empathic and Self-Regulatory Processes Governing Doping Behavior. Front Psychol. 2017;8.
Smith D, Rutty MC, Olrich TW. Muscle dysmorphia and anabolic-androgenic steroid use. In: Hall M, Grogan S, editors. Chemically modified bodies. London: Palgrave Macmillan; 2016.
Joubert HE, Melluish S. Considering anabolic androgenic steroid use in relation to non-substance related diagnostic categories with special emphasis on eating disorders: a systematic review. J Subst Use. 2016;21(2):210–6.
Harris MA, Dunn M, Alwyn T. A qualitative exploration of the motivations underlying anabolic-androgenic steroid use from adolescence into adulthood. Health Psychol Rep. 2016;4(4):315–20.
Greenway CW, Price C. Muscle dysmorphia and self-esteem in former and current users of anabolic-androgenic steroids. Perform Enhanc Health. 2020;7:3–4.
Greenway CW, Price C. A qualitative study of the motivations for anabolic-androgenic steroid use: the role of muscle dysmorphia and self-esteem in long-term users. Perform Enhanc Health. 2018;6(1):12–20.
Coxon J. Hypogonadism persistence after long-term illicit use of anabolic-androgenic steroids. J Sex Med. 2016;13(5):S180-S.
Mossman JA, Pacey AA. The fertility fitness paradox of anabolic-androgenic steroid abuse in men. J Intern Med. 2019;286(2):231–2.
Hibbert MP, Brett CE, Porcellato LA, Hope VD. Image and performance enhancing drug use among men who have sex with men and women who have sex with women in the UK. Int J Drug Policy. 2020:102933. https://doi.org/10.1016/j.drugpo.2020.102933.
Amaral JMX, Padilha MC, Chagas SV, Baker JS, Mullen C, Vieira Neto L, et al. Effective treatment and prevention of attempted suicide, anxiety, and aggressiveness with fluoxetine, despite proven use of androgenic anabolic steroids. Drug Test Anal. 2021;13(1):197–202.
Woodward C, Smith J, Acreman D, Kumar N. Hepatocellular carcinoma in body builders; an emerging rare but serious complication of androgenic anabolic steroid use. Ann Hepatobiliary Pancreat Surg. 2019;23:174–7.
Brennan R, Wells J, Van Hout MC. “Blood letting”-Self-phlebotomy in injecting anabolic-androgenic steroids within performance and image enhancing drug (PIED) culture. Int J Drug Policy. 2018;55:47–50.
Bates G, McVeigh J. Image and performance enhancing drugs 2015 survey results. Liverpool: Centre for Public Health: Liverpool John Moores University; 2016.
Gilmore H, Shannon S, Leavey G, Dempster M, Gallagher S, Breslin G. Help-seeking beliefs among anabolic androgenic steroid users experiencing side effects: an interpretive phenomenological analysis. J Clin Sport Psychol. 2020;14(4):359–75.
Hope V, Leavey G, Morgan G, Acreman D, Turmer D, Smith J. Facilitators and barriers to health care access amongst people using image and performance enhancing drugs in wales: findings & outcomes. Cardiff: Public Health Wales; 2020.
Mulrooney KJ, van de Ven K, McVeigh J, Collins R. Commentary: Steroid Madness- has the dark side of anabolic-androgenic steroids (AAS) been over-stated? Perform Enhanc Health. 2019;6(3–4):98–102.
McVeigh J. Engaging with people who use image and performance enhancing drugs: One size does not fit all. Int J Drug Policy. 2019;71:1–2.
Zahnow R, McVeigh J, Ferris J, Winstock A. Adverse effects, health service engagement, and service satisfaction among anabolic androgenic steroid users. Contemp Drug Probl. 2017;44(1):69–83.
Henning A, Andreasson J. Preventing, producing, or reducing harm? Fitness doping risk and enabling environments. Drugs Educ Prev Policy. 2020:1–10. https://doi.org/10.1080/09687637.2020.1865273.
Hill SA, Waring WS. Pharmacological effects and safety monitoring of anabolic androgenic steroid use: differing perceptions between users and healthcare professionals. Ther Adv Drug Saf. 2019;10:2042098619855291.
Harvey O, Parrish M, van Teijlingen E, Trenoweth S. Support for non-prescribed anabolic androgenic steroids users: a qualitative exploration of their needs. Drug-Educ Prev Polic. 2020;27(5):377–86.
Harvey O, Parrish M. Social work implications of anabolic-androgenic steroid use, particularly among young people: a literature review. Practice. 2019;32(3):209–28.
Harvey O. ‘Shades of Grey’: the ethics of social work practice in relation to un-prescribed anabolic androgenic steroid use. Practice. 2018;31(4):239–58.
SDF Working Group on IPEDS. Image and Performance Enhancing Drugs (IPEDS) in Scotland. SDF; 2018.
Miller R. Building Bodies: Investigating Image and Performance Enhancing Drugs (IPEDs) Use in Scotland. Edinburgh: Scottish Government; 2017.
Iversen J, Hope VD, McVeigh J. Access to needle and syringe programs by people who inject image and performance enhancing drugs. Int J Drug Policy. 2016;31:199–200.
McVeigh J, Kimergard A, Bates G, Hope VD, Ncube F. Harm reduction interventions should encompass people who inject image and performance enhancing drugs. BMJ. 2016;353:i1889.
Bates G, Backhouse S. Preventing image and performance enhancing drug use: it’s not all chalk and talk. In: Van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Bates G, Begley E, Tod D, Jones L, Leavey C, McVeigh J. A systematic review investigating the behaviour change strategies in interventions to prevent misuse of anabolic steroids. J Health Psychol. 2019;24(11):1595–612.
Brennan R, Wells JSG, Van Hout MC. “Beauty through the eye of a needle”—an online study of the practices and beliefs of people who inject performance and image enhancing drugs (PIEDs). In: Van de Ven K, Mulrooney K, McVeigh J, editors. Human enhancement drugs. Abingdon: Routledge; 2019.
Mullen C, Whalley BJ, Schifano F, Baker JS. Anabolic androgenic steroid abuse in the United Kingdom: an update. Br J Pharmacol. 2020;177(10):2180–98.
Harvey O, Keen S, Parrish M, van Teijlingen E. Support for people who use Anabolic Androgenic Steroids: A Systematic Scoping Review into what they want and what they access. BMC Public Health. 2019;19(1):1024.
Glass R, Hope VD, Njoroge J, Edmundson C, Smith J, McVeigh J, et al. Secondary distribution of injecting equipment obtained from needle and syringe programmes by people injecting image and performance enhancing drugs: England and Wales, 2012–15. Drug Alcohol Depend. 2019;195:40–4.
Hope VD, McVeigh J, Begley E, Glass R, Edmundson C, Heinsbroek E, et al. Factors associated with hepatitis C and HIV testing uptake among men who inject image and performance enhancing drugs. Drug Alcohol Rev. 2020;40(4):586–96.
Brennan R, Wells JSG, Van Hout MC. The injecting use of image and performance-enhancing drugs (IPED) in the general population: a systematic review. Health Soc Care Community. 2017;25(5):1459–531.
Brennan R, Wells JSG, Van Hout MC. “Raw juicing” – an online study of the home manufacture of anabolic androgenic steroids (AAS) for injection in contemporary performance and image enhancement (PIED) culture. Perform Enhanc Health. 2018;6(1):21–7.
Edwards C, Tod D, Molnar G, Markland D. Predicting muscularity-related behavior, emotions, and cognitions in men: The role of psychological need thwarting, drive for muscularity, and mesomorphic internalization. Body Image. 2016;18:108–12.
Cranswick I. Beyond the muscles: exploring the meaning and role of muscularity in identity. Liverpool: Liverpool John Moores University; 2019.
Hope VD, McVeigh J, Smith J, Glass R, Njoroge J, Tanner C, et al. Low levels of hepatitis C diagnosis and testing uptake among people who inject image and performance enhancing drugs in England and Wales, 2012–15. Drug Alcohol Depend. 2017;179:83–6.
Bates G, Hope V, McVeigh J. HIV among people using anabolic steroids in the United Kingdom: an overview. HIV Nursing: Sharing best practice in HIV care. 2017;17(20-23).
Acknowledgements
The authors would like to thank the members of both the Study Steering Committee and the Public Expert Advisory Board for their advice and support throughout this project.
Funding
The research was funded by the NIHR, grant holder Professor Jim McVeigh under grant number NIHR132730. The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS or the UK Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
All authors read and approved the final manuscript.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table 2
. Charted Records of United Kingdom publications on anabolic androgenic steroids and associated IPED use (2016-2020).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
McVeigh, J., Hearne, E., Boardley, I. et al. Generating evidence on the use of Image and performance enhancing drugs in the UK: results from a scoping review and expert consultation by the Anabolic Steroid UK network. Harm Reduct J 18, 107 (2021). https://doi.org/10.1186/s12954-021-00550-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12954-021-00550-z